On the occasion of the International Day for Maternal Health and Rights on 11 April, PMNCH stresses the multitude effects of the pandemic, which has interrupted movement of crucial medical supplies, diverted the health workforce and disrupted health services, causing reduction in service coverage for pregnant women and newborns.
In response, PMNCH issued a 7-point Call to Action on COVID-19 to advocate for urgent action to respond to the devastating effects of the pandemic on the health of women, children, and adolescents, as well as the societies and economies that support them.
The first ask of this Call to Action is particularly relevant today, urging governments:
To ensure sexual, reproductive, maternal, newborn, child, and adolescent health (SRMNCAH) services, supplies and information, and demand generation including for contraception, safe abortion, immunization, safe delivery, stillbirth prevention, and mental health are upheld.
Maintaining essential services
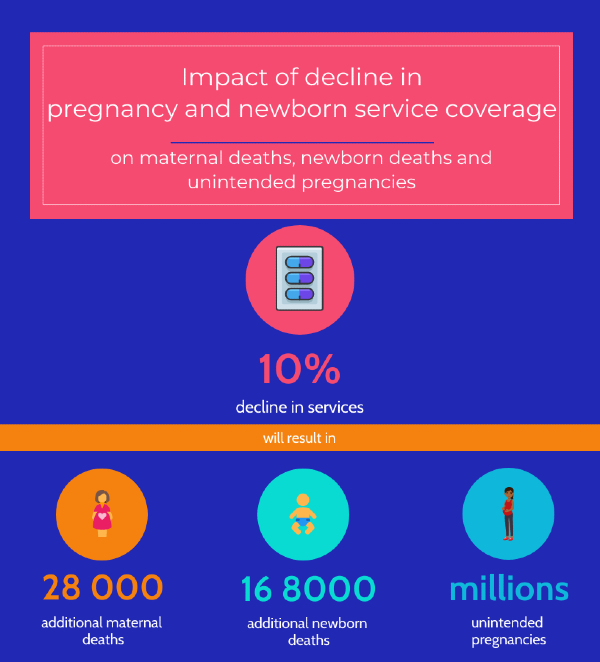
Maternal and newborn child mortality rates are expected to increase due to disruptions caused by COVID-19. WHO recommends that pregnancy and newborn health services are maintained. Early estimates suggested that even a modest decline of 10% in pregnancy and newborn service coverage would result in an additional 28 000 maternal deaths, 168 000 newborn deaths, and millions of unintended pregnancies1.
Maintaining quality care during and after pregnancy is crucial to preventing death and disability. For example, a reduction in administration of parenteral medicines, such as uterotonics and antibiotics would result in 60% more maternal deaths, while a drop in antibiotics for pneumonia and neonatal sepsis and of oral rehydration solution for diarrhoea would account for 41% additional child deaths2.

Keeping mothers and babies together
Close contact and early, exclusive breastfeeding help a baby thrive!
There is no evidence of transmission of the virus responsible for COVID-19 passing from mothers to babies during pregnancy or delivery, nor is there evidence of infection through breastmilk. Mothers should be supported to breastfeed with good respiratory hygiene, hold newborns skin-to-skin, and share a room with the baby.
Q&A on pregnancy and childbirth
The benefits of keeping the mother and baby together far outweigh the potential risk of COVID-19 infection. However, due to the fear of contracting the disease, many small and vulnerable newborns do not benefit from Kangaroo Mother Care (KMC), a life-saving method involving skin-to-skin contact.
A new analysis found that the benefits of KMC is 65-fold higher than the mortality risk of COVID-193. This trend is particularly alarming in low and middle-income countries. The results of a global survey from 1120 respondents in 62 countries found that two-thirds of health care professionals did not support KMC and exclusive breastfeeding for mothers with unknown or positive COVID-19 status due to poor preparedness and guidelines 4. Half of the time, newborns were separated from their COVID-positive mothers, and 16% of the time for those with unknown status. The follow-up consultations to health facilities also dived by 73% because of families’ fear to visit hospitals.
Breastfeeding and close contact continue being critical during COVID-19
Breastfeeding should also be supported during the pandemic, for mothers wishing to practice it. A recent analysis found that if mothers with confirmed infection are recommended to avoid or stop breastfeeding more infant deaths would be expected –the risks of avoiding or stopping breastfeeding outweigh any perceived potential benefits5.
COVID-positive new mothers can breastfeed, if they practice respiratory hygiene by wearing a mask, washing hands before and after touching the baby, and cleaning the surfaces.
If a COVID-positive mother is too unwell to breastfeed, she can be supported in other ways by expressing milk, relactation and using donor human milk.
Our response to the COVID-19 pandemic now will shape how we tackle epidemics in the future.
Explore PMNCH COVID-19 and WCAH toolkits

Care for small and sick newborns during COVID-19

1 Riley T, Sully E, Ahmed Z, Biddlecom A. Estimates of the Potential Impact of the COVID-19 Pandemic on Sexual and Reproductive Health In Low- and Middle-Income Countries. Int Perspect Sex Reprod Health. 2020 Apr 16;46:73-76. doi: 10.1363/46e9020. PMID: 32343244.
2 Roberton T, Carter ED, Chou VB et al. Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: a modelling study. Lancet Glob Health. 2020; 8:e901–e908. doi: 10.1016/S2214-109X(20)30229-1
3 Minckas N, Medvedev MM, Adejuyigbe EA et al. Preterm care during the COVID-19 pandemic: A comparative risk analysis of neonatal deaths averted by kangaroo mother care versus mortality due to SARS-CoV-2 infection. Lancet Glob Health. 2021. doi: /10.1016/j.eclinm.2021.100733
4 Rao SPN, Minckas N, Medvedev MM, Gathara D, Y N P, et al. COVID-19 Small and Sick Newborn Care Collaborative Group. Small and sick newborn care during the COVID-19 pandemic: global survey and thematic analysis of healthcare providers' voices and experiences. BMJ Glob Health. 2021 Mar;6(3):e004347. doi: 10.1136/bmjgh-2020-004347. PMID: 33716220; PMCID: PMC7959239
5 Rollins N, Minckas N, Jehan F, Lodha R, et al. WHO COVID-19 Maternal, Newborn, Child and Adolescent Health Research Network, Newborn and Infant Feeding Working Groups. A public health approach for deciding policy on infant feeding and mother-infant contact in the context of COVID-19. Lancet Glob Health. 2021 Apr;9(4):e552-e557. doi: 10.1016/S2214-109X(20)30538-6. Epub 2021 Feb 22. PMID: 33631131; PMCID: PMC7906661

.png?sfvrsn=6d0e27cd_1)



